You don’t need google to tell you that CANCER is still one of the leading global health concerns along with CVDs or cardiovascular diseases, and it has been for the longest time.
But CANCER is not a single disease, it is in fact a group of diseases characterized by the uncontrolled growth and division of abnormal cells in the body. Cancer has most likely existed for as long as multicellular life forms have been around because it involves a fundamental disruption of cell growth and regulation, which are essential processes for complex organisms like humans.
Cancer
The earliest documented descriptions of cancer date back to ancient civilizations. The term “cancer” itself comes from the Greek word “karkinos,” which was used by the physician Hippocrates (circa 460-370 BCE) to describe tumors and growths. In ancient Egypt, there are references to tumors and growths in medical texts that date back to around 1600 BCE.
However, our understanding of cancer and its causes has evolved significantly over the centuries. Early civilizations often attributed cancer to supernatural causes, and treatments were often ineffective and sometimes harmful.
It was not until the development of modern medical and scientific methods in the 19th and 20th centuries that our understanding of cancer began to advance significantly. The discovery of the role of genetics and cellular biology in cancer, as well as the identification of risk factors such as tobacco use and exposure to carcinogens, has contributed to our modern understanding of the disease.
In the 20th century, significant progress was made in cancer research and treatment, including the development of chemotherapy, radiation therapy, and surgical techniques. Cancer research continues to advance rapidly, with ongoing efforts to better understand the molecular and genetic mechanisms underlying cancer and to develop more effective treatments and prevention strategies.
Just recently, a media forum on the evolving landscape of cancer treatments was held at the New World Hotel with insights from Dr Tanujaa Rajasekaran, a Senior Consultant, Medical Oncologist at Parkway Cancer Centre.
Dr. Tanujaa Rajasekaran

Dr Tanujaa has expertise in general medical oncology, with subspecialty interests in the management of lung, genitourinary, head and neck cancers and geriatric oncology.
Prior to joining Parkway Cancer Centre, Dr Tanujaa served as a Consultant at National Cancer Centre Singapore and as the Medical Director of the Changi General Hospital oncology unit.
She graduated from National University of Singapore (NUS) and was awarded the Dean’s list during her undergraduate studies in 2006. Thereafter, she obtained her postgraduate qualifications – Masters of Medicine (Internal Medicine) from NUS, and her Membership of the Royal College of Physicians (UK). Subsequently, she went on to complete her specialist training in Medical Oncology in the National Cancer Centre Singapore.
Dr Tanujaa is also actively involved in medical education. She was a core faculty member of the Medical Oncology Senior Residency Program, as well as a Clinical lecturer at Yong Loo Lin School of Medicine, NUS. She was also an Assistant Professor at Duke NUS medical school. She has also published in a number of internationally renowned journals. Dr Tanujaa is a member of several professional bodies, including the American Society of Clinical Oncology (ASCO), European Society of Medical Oncology (ESMO) and International Society of Geriatric Oncology (SIOG). She is also Singapore’s National representative for SIOG.
Dr Tanujaa Rajasekaran has received numerous awards including Singapore Health Quality Service Awards in 2019 and 2022 as well as the European Society of Medical Oncology (ESMO) fellowship grant for her research in geriatric oncology.
The Evolving Landscape of Cancer Treatments
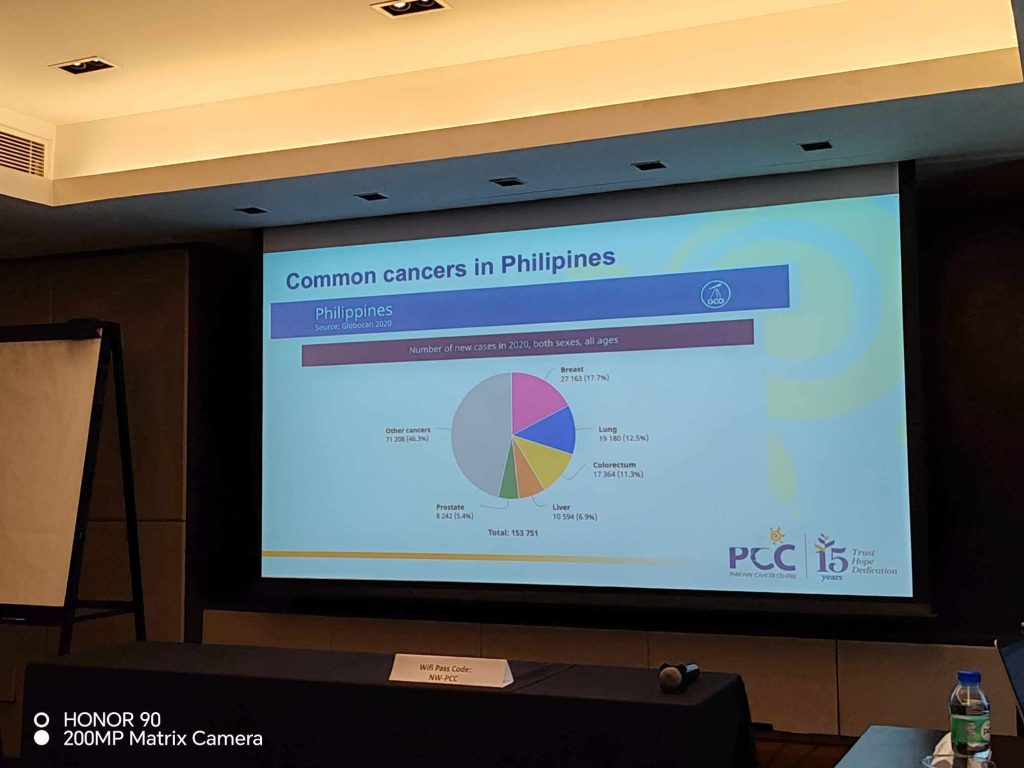
Before her presentation, Dr Tanujaa gave us an a five key point overview of the current situation of cancer in the world (and the Philippines).

- Cancer is an uncontrolled growth of abnormal cells
- Cancers grow and then spread
- Lifetime risk of developing a cancer is now at 40%
- Risk of dying from cancer is now at 20%
- The most common cancer in the Philippines is Breast Cancer (17.7%), followed by Lung Cancer (12.5%), Colorectum Cancer (11.3%), Liver Cancer (6.9%) and Prostate Cancer (5.4%).
Cancer can develop in virtually any part of the body, and there are over 100 different types of cancer, each with its own characteristics and behaviors. The specific causes of cancer can vary, but they often involve genetic mutations or changes that disrupt the normal regulation of cell growth and division. Some common risk factors for cancer include exposure to carcinogens (cancer-causing substances), genetics, lifestyle factors (such as smoking, diet, and physical activity), and certain infections.
Early detection and treatment are crucial for improving the prognosis and outcomes for individuals with cancer. Treatment options for cancer may include surgery, radiation therapy, chemotherapy, immunotherapy, targeted therapy, hormone therapy, and stem cell transplant, among others. The choice of treatment depends on the type and stage of cancer, as well as the individual’s overall health and preferences. Dr Tanujaa calls this as a multidisciplinary care in cancer.

To put it in perspective, there are four areas of systemic treatments available right now in medical oncology:
- Chemotherapy
- Hormonal Therapy
- Targeted Therapy
- Immunotherapy
Dr Tanujaa highlighted several breakthrough treatments which include Immune Checkpoint Inhibitors, CAR-T cell Therapy and Photon Therapy.
Immune Checkpoint Inhibitors
Immune checkpoint inhibitors are a type of treatment that works by harnessing the body’s own immune system to target and attack cancer cells. To understand how immune checkpoint inhibitors work, it’s important to know a bit about the immune system and the role of checkpoints in regulating immune responses.
The immune system has several mechanisms to identify and eliminate abnormal or foreign cells, including cancer cells. T cells are a type of immune cell that plays a central role in this process. When T cells encounter a potential threat, such as a virus-infected cell or a cancer cell, they are activated to attack and destroy the target.
However, to prevent the immune system from attacking healthy cells and causing autoimmune reactions, there are built-in regulatory mechanisms known as immune checkpoints. Immune checkpoint proteins, such as CTLA-4 (Cytotoxic T-Lymphocyte-Associated Protein 4) and PD-1 (Programmed Cell Death Protein 1), help regulate the immune response by sending signals that can either activate or inhibit T cell activity.
Cancer cells can take advantage of these immune checkpoints to evade detection and attack by the immune system. They may express proteins like PD-L1 (Programmed Death-Ligand 1), which binds to PD-1 on T cells, sending an inhibitory signal that “turns off” the T cells and prevents them from attacking the cancer cells. This allows cancer cells to avoid immune destruction and continue growing unchecked.
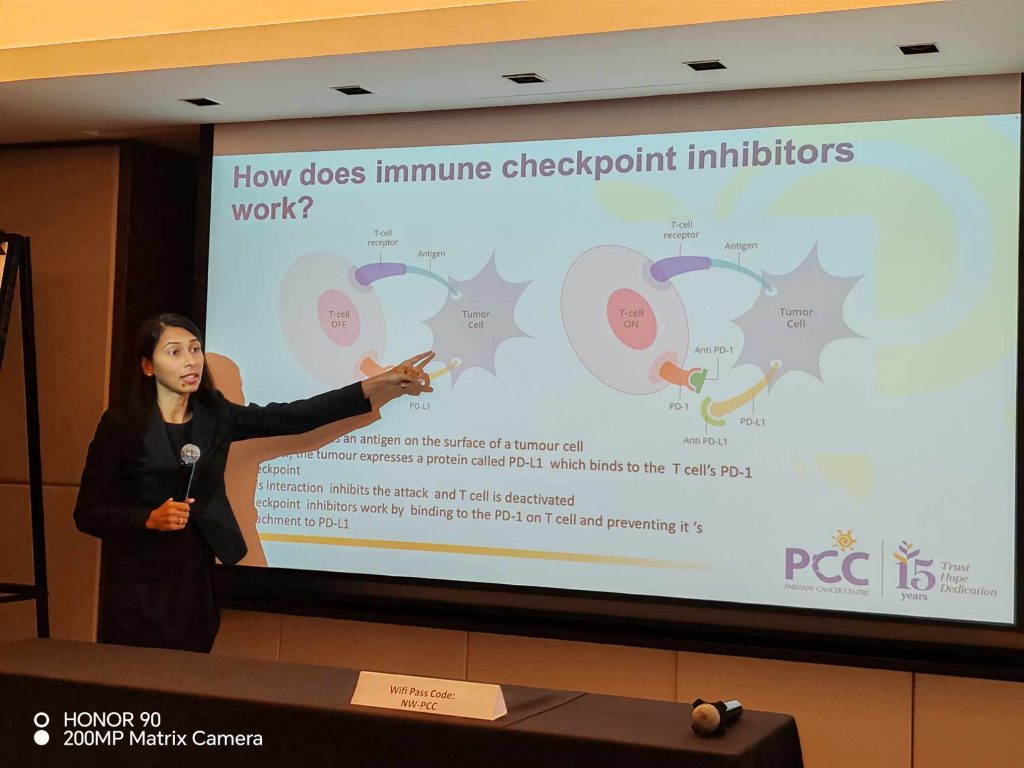
Immune checkpoint inhibitors work by blocking these inhibitory signals and reactivating the T cells to attack cancer cells. Here’s how they operate:
Blockade of Immune Checkpoints: Immune checkpoint inhibitors are monoclonal antibodies (drugs) that target specific immune checkpoint proteins. For example, drugs like pembrolizumab and nivolumab target PD-1, while drugs like ipilimumab target CTLA-4. By binding to these checkpoint proteins, the inhibitors prevent them from interacting with their ligands on cancer cells.
Activation of T Cells: By blocking the immune checkpoints, T cells are released from inhibition and become reactivated. They can now recognize and attack cancer cells as they should.
Immune Response Against Cancer: With the immune system no longer inhibited, a robust immune response is mounted against the cancer cells. T cells infiltrate the tumor and work to destroy cancer cells throughout the body.
It’s important to note that not all patients respond to immune checkpoint inhibitors, and their effectiveness can vary depending on the type of cancer and the individual’s immune system. Researchers continue to study these treatments and explore ways to improve their efficacy, including combinations with other therapies.
Immune checkpoint inhibitors have shown remarkable success in certain cancers, such as melanoma, non-small cell lung cancer, and some types of lymphoma, leading to durable responses and even long-term remission in some cases. However, they can also have side effects related to overactivation of the immune system, which need to be carefully managed by healthcare professionals during treatment.
CAR-T Cell Therapy
CAR-T cell therapy (Chimeric Antigen Receptor T-cell therapy) is a groundbreaking and innovative approach to cancer treatment. It’s a form of immunotherapy that involves genetically modifying a patient’s own T cells (a type of immune cell) to target and destroy cancer cells. CAR-T cell therapy has shown remarkable success in treating certain types of blood cancers and is considered a significant advancement in the field of oncology.
Here’s how CAR-T cell therapy works:
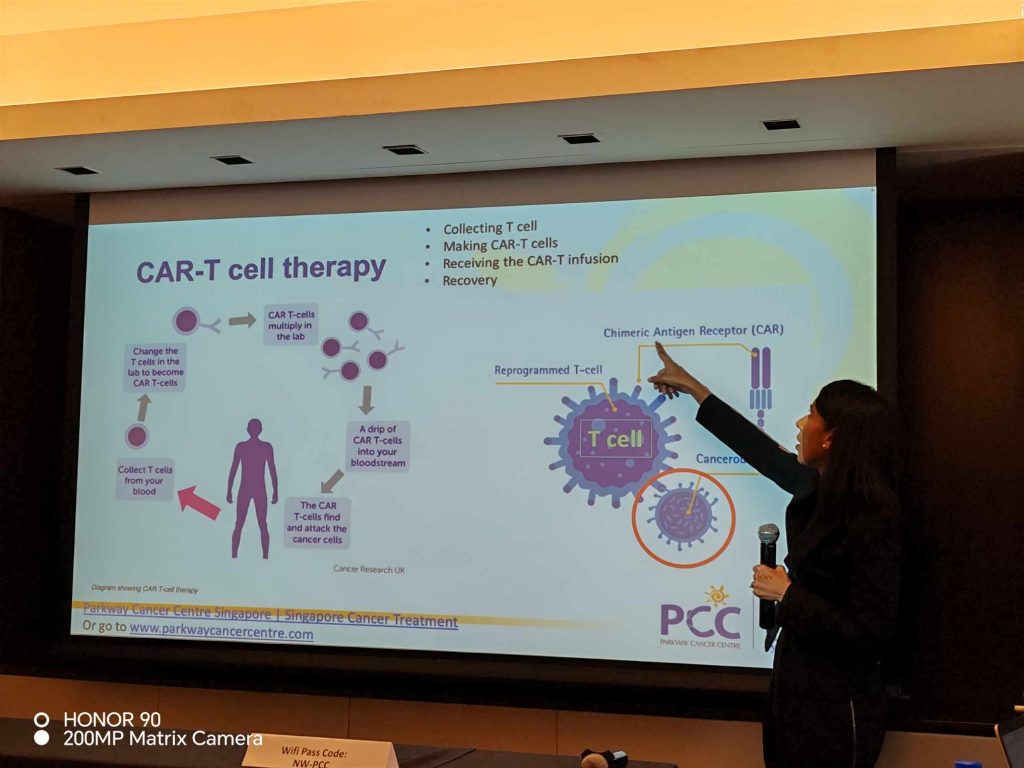
Collection of T Cells: First, T cells are extracted from the patient’s blood through a process called leukapheresis. This is similar to donating blood but specifically targets T cells.
Genetic Modification: In a laboratory, the extracted T cells are genetically engineered to express a chimeric antigen receptor (CAR) on their surface. This receptor is designed to recognize a specific protein or antigen found on the surface of cancer cells. The CAR is a synthetic construct that combines the binding domain of an antibody with signaling domains from T-cell receptors.
Expansion and Activation: The modified CAR-T cells are then cultured and expanded in large numbers. This process typically takes a few weeks. During this time, the CAR-T cells are activated and prepared for infusion back into the patient.
Infusion: Once a sufficient number of CAR-T cells have been generated, they are infused back into the patient’s bloodstream through an intravenous (IV) infusion. This infusion is a one-time treatment.
Targeting and Destruction of Cancer Cells: The CAR-T cells circulate in the patient’s body and, when they encounter cancer cells that express the specific antigen targeted by the CAR, they bind to those cells. Once bound, the CAR-T cells become activated and initiate a potent immune response against the cancer cells, leading to their destruction.
CAR-T cell therapy has shown remarkable success, particularly in the treatment of B-cell malignancies like acute lymphoblastic leukemia (ALL), chronic lymphocytic leukemia (CLL), and certain types of non-Hodgkin lymphoma (NHL). Some patients who had no other effective treatment options have experienced complete and durable remissions after CAR-T cell therapy.
However, CAR-T cell therapy can have significant side effects, including cytokine release syndrome (CRS) and neurological toxicity, which can be severe but are generally manageable with appropriate medical care. Researchers are continually working to refine and expand the use of CAR-T cell therapy to treat other types of cancer and improve its safety and effectiveness.
It’s important to note that CAR-T cell therapy is a highly specialized and personalized treatment that is currently approved for specific types of cancer in certain patient populations. Its use is determined on a case-by-case basis, and patients should consult with their oncologists to determine if it’s a suitable option for their specific condition.
Photon Therapy
Photon therapy is an advanced and highly precise radiation treatment to destroy tumor cells. It delivers minimal entrance radiation and no radiation beyond the intended tumor as compared to traditional radiation (photon) therapy.
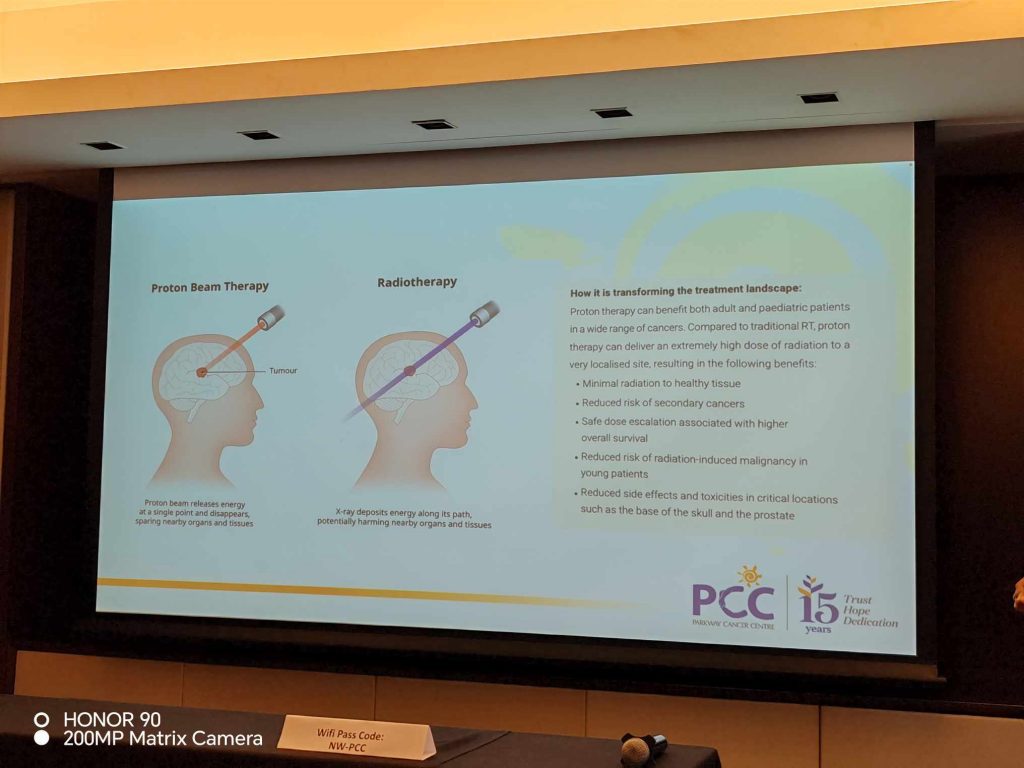
Photon Beams: In photon therapy, the high-energy radiation is typically delivered using a medical device called a linear accelerator (LINAC). This machine generates photon beams, which are streams of high-energy X-rays or gamma rays. These photon beams are directed precisely at the tumor site.
Precise Targeting: One of the advantages of photon therapy is its ability to precisely target the tumor while minimizing damage to surrounding healthy tissues. Radiation oncologists use advanced imaging techniques (such as CT scans or MRI) to create a treatment plan that ensures the radiation is delivered with accuracy and precision.
Fractionation: Radiation therapy is often delivered in multiple sessions or fractions over a period of days or weeks. This approach, known as fractionation, allows for the effective destruction of cancer cells while giving healthy tissues time to repair between treatments. The treatment is typically delivered within 5 minutes, 5 days a week and up to 8 weeks. The procedure is usually painless and done in an outpatient setting.
Types of Photon Therapy: There are different techniques within photon therapy, including intensity-modulated radiation therapy (IMRT), volumetric modulated arc therapy (VMAT), and stereotactic body radiation therapy (SBRT), among others. These techniques vary in how the radiation is shaped and delivered to the tumor.
Side Effects: Like all forms of radiation therapy, photon therapy can cause side effects, which may include fatigue, skin irritation, and changes in the treated area. The specific side effects and their severity depend on the location of the tumor and the treatment plan.
Photon therapy is a highly effective and valuable tool in the fight against cancer. It is used for a wide range of types and stages, and the treatment approach is customized for each patient. The goal is to deliver a therapeutic dose of radiation to the tumor while minimizing harm to healthy tissues and organs. Patients considering radiation therapy should consult with their oncology team to determine the most appropriate treatment plan for their specific diagnosis and medical history.
As per Dr Tanujaa’s presentation, it is worth noting that while there are many advances in the treatment of cancer, there is still no miracle cure for the disease and its reason for being is still pretty much a mystery. The cost of treatment is still very high and the most advanced treatments are still not readily available here in the Philippines. But they are however within reach or more accessible so to speak.
Parkway Cancer Center
Parkway Cancer Centre is a prominent oncology treatment facility based in Singapore. It is known for providing comprehensive care and treatment services, including diagnostics, surgery, radiation therapy, chemotherapy, and immunotherapy, among others. PCC is part of the Parkway Pantai Limited network, which is one of the largest and most well-established private healthcare providers in Asia.

Key features of Parkway Cancer Centre:
Multidisciplinary Care: The center emphasizes a multidisciplinary approach to treatment, where a team of oncologists, surgeons, radiologists, nurses, and other specialists collaborate to develop personalized treatment plans for each patient.
Advanced Technologies: PCC is equipped with state-of-the-art medical equipment and technologies, allowing for precise diagnosis and treatment of various types of cancer.
Comprehensive Services: They offer a wide range of services, including medical oncology, surgical oncology, radiation oncology, hematology, palliative care, and supportive care.
Clinical Trials: PCC is involved in clinical research and may offer eligible patients access to clinical trials and experimental treatments.
Patient-Centered Care: The center prioritizes patient comfort and well-being, providing a supportive and compassionate environment for individuals and their families facing cancer.
International Patient Services: Given its reputation and location in Singapore, Parkway Cancer Centre also serves international patients who seek high-quality care.
HOPE
During her presentation, Dr Tanujaa shared the inspiring story of pro-cyclist Lance Armstrong:
- Armstrong was diagnosed with Stage 3 testicular cancer at age 25
- He had metastatic disease to his brain and lungs
- He was then cured with chemotherapy
- He then went on to win seven consecutive Tour de France from 1999 to 2005
Yes, we CAN HOPE and WIN our fight against cancer!
- Taiwan at the Forefront of Green Economy - July 26, 2024
- Discover Tohoku in the Summer - July 25, 2024
- Back-to-School Tips: How to Make the Most of What You Already Have - July 25, 2024